DISTINCT CHALLENGE, UNIQUE OPPORTUNITY
Hospital leaders are used to thinking of the supply chain as a major cost center. But when it comes to the perioperative supply chain, focusing exclusively on cost is a mistake. A successful hospital OR is a carefully balanced system of providers, workflows, and materials. Every component of the system can have a major impact on overall results. In this environment, supplies and equipment are not just a source of cost, they are a key driver of operational efficiency, provider satisfaction, clinical quality, and patient outcomes. To ensure a high-performing OR, hospital leaders must take a strategic approach to managing the perioperative supply chain. Surgical Directions has worked with hospitals nationwide to align perioperative supply chain processes with OR operations and financial goals. In our experience, implementing a strategic supply chain initiative can realize an initial reduction in direct costs of 3% or more. Just as important, a strategic approach to the supply chain can increase operational efficiency and support OR strategy by strengthening links with key surgeon staff.
SET THE STAGE FOR DATA-BASED MANAGEMENT
The first step is to take full advantage of technology to manage the perioperative supply chain. While technology is pervasive in healthcare, most hospital ORs still rely heavily on manual systems for handling and tracking materials. The good news is that supply chain leaders can build an effective OR data platform using existing IT resources. Three components are key:
- An accurate master item file In most hospitals, the master item file is mainly used as a tool for managing the purchasing process. In high-performing hospitals, however, supply chain leaders use the master file to get a comprehensive view of supply utilization. The key is to establish processes to ensure the master file is accurate, with minimal use
of miscellaneous charge codes, and continuously up to date. Staff should not only add any new products but also record changes to existing products, such as changes in code, price, case quantity, shipping fees, etc. This allows supply chain leaders to use the master item file to track products throughout the system and accurately calculate product costs. - Full charge capture Many hospital ORs do not charge for items under a certain price threshold (for example, $20). However, failing to capture use an item means that it cannot be tied to a case, used to calculate the cost of a surgical procedure, or allow automatic supply replenishment. OR leaders should establish a supply capture validation process regardless of cost or whether it is charged to the patient. OR staff should have the ability to capture every item opened, both on the preference card as well as additional items.
- Fully implemented digital tools Almost all hospitals have a range of digital tools for managing supply inventories. However, many ORs do not take full advantage of their existing capabilities
to automate inventory management. First, determine which storeroom management tools are available. Many hospitals have already invested in barcoding systems that can be effectively adapted to the OR. In addition, assess the OR’s existing inventory management software for unused capabilities. Many software systems can automate tasks such as monitoring expirations.
OPTIMIZE EVERY LINK IN THE PERIOPERATIVE SUPPLY CHAIN
The information platform described in the previous page (accurate master file, full charge capture, and fully leveraged software) will automatically create efficiencies. More importantly, it will give OR and supply chain leaders a comprehensive view of how products move throughout perioperative services. The leadership team can use this data to pursue advanced cost control opportunities and align the perioperative supply chain with operational and strategic goals. Focus on the following key priorities:
Leverage the system to establish rational par levels
Oftentimes stockouts and overages occur for many OR supply categories. Accurate utilization data enable OR leaders, in collaboration with OR stock replenishment staff, to establish minimum and maximum stock levels based on actual demand. Setting rational par levels for key supplies can significantly reduce inventory on hand and increase annual turnover.
Optimize supply locations and logistics
In many hospitals, OR storerooms are crowded with supplies, instrument trays, and equipment, and more distant storage areas are poorly organized. In the same way that utilization data can help OR leaders set rational par levels, it can also help procedural area leaders identify true supply needs. This allows materials management to create effective distribution and storage strategies for every department. In general, supplies for emergent needs should be close at hand. Many other supplies can be stored where case carts are picked. Redundant stocks should be kept to a minimum. The overall goal is to create a system that delivers the right product at the right time for the right procedure.
Optimize product selection for operational efficiency
Supply utilization data can also be used to make informed decisions about how product selection impacts department operations. For example, an OR may stock several different types of electrosurgical (ESU) devices and disposables. Standardizing ESU devices streamlines equipment setup, operation, and maintenance processes. This allows staff to become more familiar with the equipment, reducing the learning curve and promoting efficient usage. Consolidating purchases of ESU disposables can result in cost savings through volume discounts, incentives, and decreased inventory on the shelf. When considering the standardization of a surgeon preference item, it is essential to involve key stakeholders, such as surgeons, OR staff, biomedical engineers, and supply chain experts. Collaborating with these stakeholders helps ensure that the standardized device meets the specific needs of the provider and the department. An accurate view of supply expenses helps supply chain and OR leaders understand the important aspects of financial management and operational efficiency. It also enables a transparent decision processes that nurses can understand and contribute to. Data-driven decisions can bring numerous benefits, including improved efficiency, cost savings, and enhanced patient safety.
Identify and pursue contracting opportunities
Supply usage data will typically reveal unrealized opportunities to benefit from bulk pricing. For example, data may show that an OR’s annual spending on surgical stapling systems is much higher than expected. Consolidating this spend to a single supplier could qualify the hospital for a better pricing tier. Supply chain leaders should also take a closer look at contract terms. Some contracting issues are relatively unique to perioperative services, such as end-of-life products. Vendors frequently introduce new products that make the same vendor’s older products obsolete — for example, a new laparoscopic system that will no longer accept legacy disposables. Even when an older product is not (strictly speaking) unusable, the introduction of a new product tends to shift surgeon preferences away from older versions. Leverage OR supply chain usage reports to identify the OR’s total exposure to end-of-life losses and negotiate an effective “return clause” when supplier contracts come up for renewal.
Examine non-stock ordering
Supply chain leaders should take a close look at their approach to stock versus non-stock purchasing. These are typically special products such as surgical meshes and bone implants. While order volumes are low, these purchases generally involve additional stock charges and transportation fees. Non-stock orders also require greater oversight from purchasing staff. Supply chain leaders should leverage utilization data to identify frequently used non-stock items that can be converted to standard inventory.
Leverage preference cards to trim waste
Another benefit of maintaining an accurate master file list is to support accurate surgeon preference cards. This allows supply chain leaders to engage in useful discussions with surgeons about supply utilization. For example, a surgeon’s preference card for urologic surgery may include a wide range of disposable supplies. However, data may show that the surgeon uses certain disposable items in less than one out of ten cases.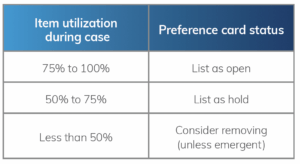
Removing these products from the preference card will help reduce inventory levels, reduce the risk of waste, and streamline the case picking process. Here is one approach to assessing preference card items:

Use cost-of-case data to engage surgeons
In today’s ultra-competitive surgeon recruitment market, many hospitals allow surgeon preferences to control spending on high-cost supplies. Accurate cost-per-case data enables supply chain leaders to engage surgeons in cost control efforts. For example, data might show that the cost-per-case for knee arthroplasty varies widely by orthopedic surgeons. What are the most efficient surgeons doing that keeps their costs low? Work with these specialists to understand their supply choices and practice patterns, and then use those results to drive discussions with other orthopedic surgeons. This approach can allow the OR to reduce its spend on high-price implants through a process led by the most respected members of the surgeon staff.
Advanced Strategy:
Use OR Analytics to Finetune Supply Chain Processes Top-performing ORs are using perioperative information systems to create highly efficient supply chain strategies. For example, the Merlin perioperative management system (developed by Surgical Directions) analyzes OR data to accurately predict case volumes by procedure, day, hour, and other parameters. This allows OR leaders to tailor re-order points for cost-efficiency. For example, the movement of disposable products can be timed to match predicted peaks in orthopedic cases.
Learn more about Merlin.
MANAGE SUPPLY CHAIN PERFORMANCE STRATEGICALLY
Like any strategic initiative in healthcare, strategic supply chain management is not a “set it and forget it” project. After implementing changes in inventory management, contracting strategy, and product selection, it is important to establish KPIs for the perioperative supply chain and monitor ongoing performance. Standard KPIs include OR inventory turnover and contract compliance. We also recommend monitoring back orders and stockouts (often a significant source of frustration for surgeons and staff), expiration rates and inventory discrepancies (indications of problems with inventory controls), and utilization of miscellaneous charge codes (an early warning sign that charging systems are falling short). In addition, OR leaders should work with the supply chain team to create a high-functioning value analysis (VA) committee for perioperative services. Currently, most VA committees focus on controlling the entry of products into the OR; few take responsibility for how products are used once they are in the inventory. The most effective OR value committees are multidisciplinary teams that monitor supply chain KPIs, continuously reexamine purchasing strategies for high-cost items, and maintain strong relationships between all perioperative stakeholders. Strategic supply chain management is the key to building a surgical services organization that achieves excellence in quality, safety, and financial outcomes.



