How Optimizing Your Operating Room Can Significantly Reduce Anesthesia Costs
A CLEAR PROBLEM: Escalating Cost of Anesthesia Coverage
Every hospital leader knows that the cost of anesthesia coverage for surgical services is skyrocketing. Approximately 80% of hospitals now provide some level of financial support to anesthesia providers, and some organizations have seen anesthesia stipends increase up to 400% in the last two to three years. Unfortunately, the anesthesia crisis is not just a cost problem; it is also a revenue problem. The growing cost of coverage reflects the growing shortage of anesthesia providers. With both anesthesiologists and CRNAs in short supply, hospitals are increasingly unable to keep ORs open. The resulting room closures are undercutting case volume at a time when hospitals desperately need to rebuild OR revenue.
A HIDDEN CAUSE: Widespread Inefficiency in the OR
While the anesthesia crisis is being driven by a severe shortage in provider supply, coverage demand is also a major factor. The underlying mechanics are complex, but the basic issue is that inefficiency in the OR schedule inflates the need for anesthesia staff. How? Here are three common ways that OR scheduling problems negatively affect anesthesia providers:
Low primetime utilization.
Ideally, cases move in and out an OR in quick succession. In reality, most rooms experience significant non-productive time between surgeries, even during primetime hours (typically 7 a.m. to 3 p.m.). This creates problems for the anesthesia group because it is contractually obligated to cover each open room for the entire shift. Essentially, the group must staff additional FTEs to cover downtime between cases. Many surgeons prefer to start their day of surgery as early as possible and finish their last case by noon. As a result, many ORs experience a very busy morning followed by a significant drop in utilization at midday. For anesthesia groups, the impact is the same as low primetime utilization—providers need to staff the entire day, whether or not it is fully productive. Ineffective scheduling also contributes to OR instability as FTEs opt for locum roles instead, inflating staffing costs and reducing consistency in the OR.
Poorly controlled NORA demand.
The cardiac catheterization lab, imaging and endoscopy suites, and other NORA locations create internal competition for anesthesia coverage. As with the main OR schedule, NORA schedules are usually not designed with efficient anesthesia coverage in mind. In addition, their wide dispersion throughout the hospital creates significant “travel time” for anesthesia providers and may require a less efficient physician-only anesthesia model. These OR schedule inefficiencies can have a major impact on an anesthesia group’s need for financial support. The following scenario illustrates the economics of anesthesia coverage for a large OR with approximately 60% utilization:
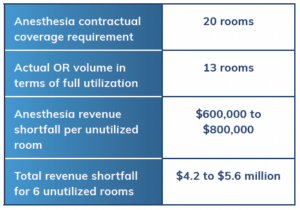
In this scenario, low OR utilization leads directly to an anesthesia stipend request starting at $4 million minimum. Clearly, inefficiency in the OR schedule is creating unsustainable anesthesia coverage costs. The good news is that any effort to optimize perioperative schedules can help reduce anesthesia costs while also improving the OR’s bottom line financial results.
AN EFFECTIVE SOLUTION: Reduce Demand for Anesthesia Coverage by Creating a More Compact Schedule
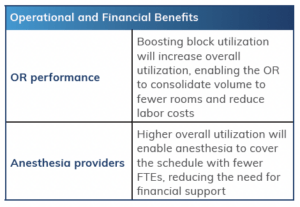
Hospital leaders have a significant opportunity to reduce anesthesia coverage costs by working toward higher utilization across perioperative services. Perioperative experts at Surgical Directions recommend focusing on three key improvements:
Eliminate “White Space” in the Surgeon Block Schedule
Many hospital ORs allocate block time to surgeons based on their seniority not their case volume or efficiency. Utilization requirements exist on the books, but they are poorly enforced. With little incentive to use their OR time efficiently, some surgeons end up with block utilization rates as low as 30%.
Clearly, OR leaders need to reform the allocation system to ensure that block time goes to the most productive surgeons. The problem is that block allocation is a politically charged issue in many hospitals, and most hospital administrators are reluctant to meddle with the status quo.
The solution: Turn the entire issue over to a governance body led by physicians themselves. A Surgical Services Executive Committee (SSEC) is essentially a “board of directors” for the OR made up of active surgeons and anesthesiologists, OR nursing leaders, and administration representatives all from within hospital.
The SSEC’s main task is to allocate block time based on actual surgeon utilization. This may mean that a surgeon with a long history in the OR—but low utilization—will see his or her block time cut back, while another surgeon who is aggressively growing a practice and using OR time efficiently will receive all the block time he or she needs.
The committee is also empowered to analyze room utilization rates and determine if fewer rooms at a higher usage rate can deliver the same volume with less staffing resources. Additionally, the committee can govern proper maintenance standards for awarding flip rooms. By understanding which surgeons most benefit from running two consecutive rooms, hospitals can add an additional option for OR optimization of space and resources to eliminate downtime while increasing productivity.
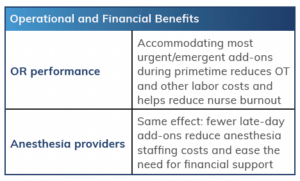
Create Special Capacity for Urgent and Emergent Cases
Many ORs block as much time as possible for elective surgery. The advantage of this strategy is to maximize capacity for high-margin elective procedures. Unfortunately, it allows limited flexibility for urgent and emergent cases. As a result, any add-on cases push the entire schedule into late afternoon or evening hours. There are several implications:
- Anesthesia must pay FTEs to cover the extended hours, increasing overall coverage costs
- The hospital must pay nurses overtime (both OR and post-anesthesia care unit (PACU) and may incur pro re nata (PRN) expenses
- Pushing cases to late afternoon and evening hours can delay admission, resulting in higher LOS
- Unreliable scheduling feeds clinician burnout and apathy towards FTE roles
The solution: Create dedicated capacity for add-on volume. Most ORs should allocate approximately 20% of the OR schedule for urgent and emergent cases; Level I trauma centers will typically require more. If volumes are high enough, consider dedicating an entire room to orthopedic trauma and/or acute care surgery. In this area, a strong SSEC can play a key role by quantifying the need and allocating the resources to accommodate unpredictable volume in an organized manner.
Integrate NORAs Locations into the Overall Schedule
To reduce the demand for anesthesia coverage, hospital leaders should ensure NORA schedules are (a) as compact as possible and (b) coordinated with the main OR schedule to avoid overall spikes in anesthesia demand. Here is the basic approach:
First, identify all anesthetizing locations in the hospital that require coverage. Major NORAs include CT and MRI units, the cardiac cath lab, the GI suite, and labor and delivery. However, there are many less prominent anesthesia needs—for example, management of invasive lines or coverage of a pain service.
Second, work with other departments and services to fit NORA demand into anesthesia availability. For example, interventional radiology (IR) may want coverage for a morning tumor ablation block, but this demand conflicts with morning room starts in the OR. The solution: Work with IR to create an afternoon block that consolidates as many cases as possible for high utilization. In addition, create agreed-upon principles for which cases merit urgent scheduling outside of the block.
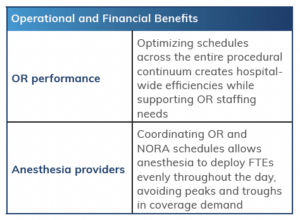
THE BOTTOM-LINE RESULTS: Comprehensive Improvement in Perioperative Services
Optimizing OR utilization can significantly reduce anesthesia’s need for financial support. This enables hospital leaders to work with anesthesia to design a strategically effective stipend agreement. Better-performing organizations have found that a “cascading stipend” can effectively align the interests of the hospital and its anesthesia providers. Ultimately, these initiatives and other improvements will help create a strong working relationship between OR leaders and their anesthesia partners and facilitate greater stability in the OR. The overall result will be more effective performance in OR quality, efficiency, and financial outcomes.