OR Payment Is Changing Rapidly
New Medicare payment models will phase in quickly over the next few years. These models will have a significant cumulative impact on surgical services revenue.
Value Based Purchasing
- The VBP program tracks several measures from the Surgical Care Improvement Project (SCIP). Surgical patient safety measures will be added in 2015.
- At risk: Hospitals can earn up to a 1% DRG bonus for high quality—or be penalized up to 1% for poor quality. The at-risk amount rises to 2% by 2017.
Readmissions Penalties
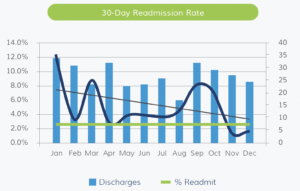
- This program currently tracks readmission rates for heart attack, heart failure and pneumonia, but it will expand to include hip and knee replacements in 2015.
- At risk: DRG penalties amount to 1% in 2013, 2% in 2014 and 3% in 2015.
Hospital-Acquired Conditions
- Bottom-quartile performers will be penalized 1% of DRG starting in 2015.
- At risk: Bottom-quartile performers will be penalized 1% of DRG starting in 2015.
Bundled Payments
- This voluntary program provides a single payment for a defined episode of care. Several program participation options include hospital inpatient services. Cost control is essential.

- At risk: High OR costs will reduce the margin on any bundled services and could result in an operating loss.
Accountable Care Organizations (ACOs)
- Shared savings mechanisms drive Medicare and private ACO programs, so cost management is critical to success. ACO entities must also meet stringent quality thresholds.

- At risk: The failure to meet quality benchmarks and control expenses will erase any shared savings and expose some ACOs to financial loss.
The New Payment Environment Demands a New OR Strategy
New payment models are a serious challenge for hospitals, but they clarify surgical services strategy. The “quality floor” is rising, while the “cost ceiling” is being lowered. Bottom line: The high-performance pathway is becoming a narrow channel.
New OR Strategy
To navigate in the new environment, hospital ORs must focus on two goals—improving quality and controlling costs.
Quality Strategy: Innovative Solutions to Improve Processes and Outcomes
Better-performing ORs have refined a handful of effective quality improvement interventions. These proven strategies strengthen processes, reduce opportunities for error and help ensure the best patient outcomes.
Optimize patients pre-operatively
One key to improving surgical quality is to ensure all patients are fully prepared for their procedure. Effective patient preparation is the result of well coordinated pre-op processes:
- Standardized scheduling: Standardized scheduling processes ensure that staff members capture complete information on the patient and the procedure.
- Testing algorithms: Standard testing requirements (based on procedure and risk factors) and evaluation guidelines help identify problems early and cost-effectively.
- Comorbidity management: Standard care protocols and pathways help staff optimize medical conditions such as diabetes and hypertension.
- Phone triage: Screening patients by phone (using a standard screening tool) allows staff to triage patients to either a normal prep timeline or a special track for high-risk patients.
Establish a “daily huddle”
Surgery requires careful coordination of providers, services and resources. But the high volume and fast pace of the typical hospital OR create many opportunities for error and poor quality. A daily huddle helps ensure that all the elements of a safe, quality surgery are in place for every patient:
- Brief daily meeting: A daily huddle typically takes place at 2 p.m. and lasts no more than 35 minutes.
- Multidisciplinary: Attendees represent anesthesia, nursing, pre-admission testing, scheduling, materials management and other key areas.
- 360° review: Participants review cases scheduled for the next day and two days forward. The review ensures that all testing is complete, all comorbidities are fully managed, any special equipment is scheduled and any unique scheduling problems have been addressed.
- Decision-making authority: The huddle group has the authority to resolve problems and issues on the spot or reschedule problematic cases.
Coordinate services through a “surgical home”
Health systems and medical groups are actively developing the medical home model to improve care coordination and outcomes in the ambulatory setting. Now, a handful of leading ORs are developing a “surgical home” concept to improve clinical outcomes, reduce costs and enhance the surgical patient experience. Key characteristics include:
- Multidisciplinary teams: management and other services work together to coordinate the perioperativ continuum of care.
- Protocol-driven: As with preoperative preparation, providers work together to develop evidence-based protocols and care pathways to optimize every point of the perioperative process—from scheduling through discharge.
Create a culture of safety
Many people think of surgical safety in terms of dramatic failures such as wrongsite surgery or retained objects. This is shortsighted. A strong culture of safety supports comprehensive improvement in quality and processes, leading to better patient outcomes across the board. Three initiatives form the foundation of surgical safety:
- Crew Resource Management (CRM): Safety techniques adapted from commercial aviation create an atmosphere of open communication and mutual respect within the hospital OR.
- WHO Surgical Safety Checklist: Implementing the WHO checklist hardwires safe practices and positive communication patterns into the surgery department.
- Just Culture: A culture of blaming keeps safety problems from coming to light. Hospital ORs that seek to create a “just culture” develop a non-punitive structure for identifying problems and weaknesses and finding effective solutions.
Cost Strategy: Proven Interventions to Control Expenses
Hospital ORs are expensive. Various estimates put OR operating expenses between $20 and $60 per minute. The bulk of these expenses are non-labor costs, which account for over 60% of most OR budgets. Better-performing ORs use a suite of proven strategies to ensure efficiency and control spending.
Control supply expenses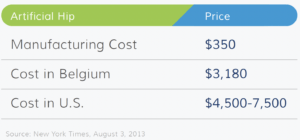
Non-labor costs represent 60% or more of the typical OR budget. Surgeon preference, supply waste and poor materials management processes all contribute to high expenses. Many ORs can reduce supply costs by 10% to 15% through a series of effective interventions:
- Effective inventory management: Most hospital ORs turn inventory just twice per year, and up to 30% of case cart items are returned unused. But better-performing ORs log 10 to 12 inventory turns per year and have a return rate of under 10%. Use the materials management information system to establish efficient par levels and reorder quantities. Create effective reorder processes and consolidate responsibilities among staff.
- Reduce clinical waste: Audit supply usage to identify frequently wasted items. Educate staff on the price of common supplies to encourage more economical practice patterns. Scrutinize custom supply packs to identify rarely used items or items that can be substituted with less expensive alternatives.
- Reduce spending on high-cost implants: Use dashboard reports to educate surgeons on the cost of their supply preferences, with comparison to Medicare reimbursement. Pay careful attention to implant preferences, and focus negotiation efforts on obtaining best-in-market prices. Renegotiate vendor agreements to hold more highcost implants on consignment.
Increase utilization through block schedule reform
Poorly designed and managed block schedules are the leading cause of low utilization within hospital ORs. Top performing departments work with surgeon leaders to develop effective block schedule rules and processes:
- Minimum block lengths: Blocks of 8 to 10 hours accommodate more cases than shorter blocks. Longer blocks also minimize downtime.
- Utilization thresholds: Effective OR schedules assign blocks to individual surgeons, not surgical groups or specialties. Individual “ownership” encourages surgeons to maintain utilization.
- Specialty-specific release: A staggered release schedule allows the OR to fill up unscheduled time while accommodating surgeon needs. For example: Cardiovascular surgery retains block time until 24 hours before, while unscheduled plastic surgery time releases 10 days out.
- Open rooms: Reserving approximately 20% of rooms for urgent and emergent cases creates flexibility and access.
Streamline patient throughput
Poor patient throughput suppresses case volume and creates a high cost structure. Leading ORs have leveraged process improvement tools and best practices to reduce downtime and make the best use of time resources.
- Reduce case times: Begin by capturing throughput time data, focusing on six key intervals—patient-in-to-prep-start, prep-start-to-prep-complete, prepcomplete-to-incision-start, incision-start-to-incision-close, incision-close-to-discharge-ready, and discharge-ready-to-patient-out. Work with surgeons, anesthesia and nursing to address the causes of excess time within each interval. For example, ORs can reduce wait time before incision by assigning a PA to complex procedures with a significant technology set-up.
- Reduced turnover times: Lean manufacturing tools such as value stream mapping can be used to identify bottlenecks, redundant processes and wasted efforts. Many ORs can use Lean methodology to reduce average turnover time by up to 70%.
Setting the Stage: 3 Prerequisites to Effective OR Transformation
Most efforts to improve surgical quality and control costs eventually run into organizational roadblocks. The biggest hurdle is physician acceptance. Without the active support of surgeons and anesthesiologists, hospital ORs cannot make measurable progress on quality and cost goals. Better-performing ORs use three physician alignment strategies to create the platform for dramatic organizational improvement.
Collaborative Governance
Top ORs establish strong physician leadership by creating a Surgical Services Executive Committee (SSEC). An SSEC is a multidisciplinary “board of directors” for the OR.
- All stakeholders: Members include clinically respected surgeons and anesthesiologists, nursing leaders, hospital senior executives and other key stakeholders.
- Strategic guidance: The SSEC’s job is to create a strategic vision for the OR, develop a formal growth strategy, sponsor process improvement and guide cultural change.
- Progressive improvement: The SSEC also functions as an operational committee for the surgery department. Hospital ORs with strong SSECs are able to achieve decisive improvements in quality, cost control and financial performance.
Data-Driven Decision Making
Physicians are trained to make decisions based on evidence. To be effective, a physician-led SSEC needs solid data to guide actions and initiatives. Better performing surgery departments commit to capturing and tracking comprehensive performance data to support organizational improvement:
- Operational metrics: Capture comprehensive measures of OR efficiency—on-time start rate, cancellation rate, average turnover time, average case time. Make sure the data can be sliced by specialty and procedure.
- Utilization metrics: Accurately calculating block time utilization is the key to enforcing block time rules. Physician dashboard reports: Provide physicians with summary metrics of their personal performance—case volume, procedure volume, plus individual quality and cost data. Advanced ORs track readmissions for individual surgeons (see below).
- Quality measures: Track quality data for individual physicians and the department as a whole. Key measure sets include Surgical Care Improvement Project (SCIP), National Surgical Quality Improvement Program (NSQIP) and National Anesthesia Clinical Outcomes Registry (NACOR).
Aligned Incentives
Successful ORs create incentives that align physicians with organizational goals in quality, safety and efficiency. This area is still evolving, but leading systems have developed two practical mechanisms:
- Incentive bonuses: Physicians who meet defined performance benchmarks in quality, efficiency, safety and patient satisfaction are eligible to share in a quality bonus pool.
- Higher reimbursement: Top healthcare systems have negotiated higher payment rates for surgeons who use their ORs. Reimbursement can be as much as 10% higher for operating at payer-designated centers ofexcellence.
Case Study: Advocate South Suburban Hospital
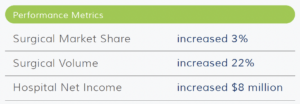
An under-performing system hospital in Chicago took steps to:
- Develop physician alignment and engagement
- Implement processes to improve quality and outcomes
- Increase overall efficiency
Situation
- Clinical performance issues
- Low operational efficiency
- Poor image among consumers
- Dependence on medical admissions
- Hospital underperforming financially
Interventions
- Established collaborative governance through SSEC Appointed new OR director
- Revamped Pre-Admission Testing
- Revised block time system and utilization rules
- Developed management/physician dashboard reports
- Implemented a daily huddle
- Cultivated a culture of safety (e.g., WHO checklist)
- Incentive structure for surgeons and anesthesiologists
Outcomes
- Most improved organization within 13-hospital system Gains in quality and outcomes (e.g., LOS decreased 11%)
- Increased surgeon satisfaction



