 Better staffing and scheduling can cut costs and help managers and directors improve the success of their business. Most departments can cut up to 10% of staffing costs without altering their ability to cover current elective, add-on and emergent case surgical cases volume.
Better staffing and scheduling can cut costs and help managers and directors improve the success of their business. Most departments can cut up to 10% of staffing costs without altering their ability to cover current elective, add-on and emergent case surgical cases volume.
Strategy surrounding the OR labor budget usually takes a back seat to block utilization and supply cost management, causing labor costs that can create significant volume to budget discrepancies. Annual labor costs (inclusive of benefits) per room include 1 Registered Nurse ($100,000/FTE) and 1 surgical technologist ($75,000/ FTE). Anesthesia staffing costs will also be affected. In many settings, the anesthesia stipend can range between $150,000 and $550,000 per room per year, depending on whether anesthesia uses a team-based or an all-physician model. Costs for nurses, surgical technologists (STs), and anesthesiologists combined are approximately $325,000 to $725,000 per room per year. Take into consideration, reducing the schedule by 2 rooms could result in annual labor expense savings of $650,000.00 and $1,450,000.00.
Most OR’s have a “horizontal” schedule, attempting to fill all rooms at 7:30 am, booking cases to follow. The department manages fluctuations in case volume by opening more rooms rather than by making the most of every available room. The number of open OR’s at the start of the day, is the primary method to staff the day, regardless of the case time scheduled within each room. Staff frequently have significant downtime during prime time OR shifts. As a result, labor costs balloon, often running 10% to 20% higher than they need to be.
The AORN staffing model is based on the number of open rooms, assuming the rooms will be used to full capacity. AORN also recommends staffing ratio’s 67% RN to 33% ST, and 67% direct, Circulating RN’s and Surgical Technologists to 33% non-direct staff, leadership, clerical and support staff.
The alternative to horizontal scheduling and the Surgical Directions recommended model is a productivity driven, “vertical” scheduling model. The number of staff required is based on several factors including, case minutes, room draw down, procedures performed, and type of facility; ASC, community, teaching, trauma center. This methodology utilizes a sliding scale of which is modified based on organizational performance and current national benchmarking.
Solutions to choose benchmark:
- Block Forecast
- Rooms Running Report
- Physical layout
- Type of procedures performed
- First case on time starts and turnaround times
- Community, teaching, trauma or ASU facility
- Room draw down plan
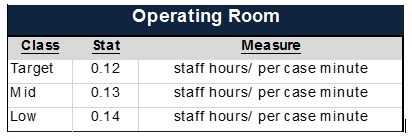
Calculate department staffing needs based on the actual case minutes, plus case turnaround time of 15 minutes, generally with a productivity factor of .12 – .14. Daily staff assignments are developed in conjunction with a rooms running report, vertical elective schedule, based on block and prime time room utilization.
A productivity driven, vertical schedule inherently minimizes downtime to make full use of staff and reduces excess staffing expense. Optimizing room utilization will typically reduce the number of staffed rooms by requiring surgeons to fill their blocks in a vertical fashion rather than scattering cases throughout the week.
As OR efficiency improves, the unused time between cases is condensed, hence staff time is optimized. Periodic staffing analysis should be completed following implementation of a block schedule redesign. Additional staff adjustment may be needed to meet the needs of the new block. In most instances there will be opportunity to realign staff, which will save the facility both in FTEs and cost. In addition a new and improved block schedule will improve efficiencies which reduce overtime and resource consumption.
Effectively managing your OR schedule and staffing model not only supports cost control, it helps keep staff engaged in your department’s mission and objectives, provides a stronger sense of ownership and consequently helps reduce staff turnover.



