Executive Summary
Introduction
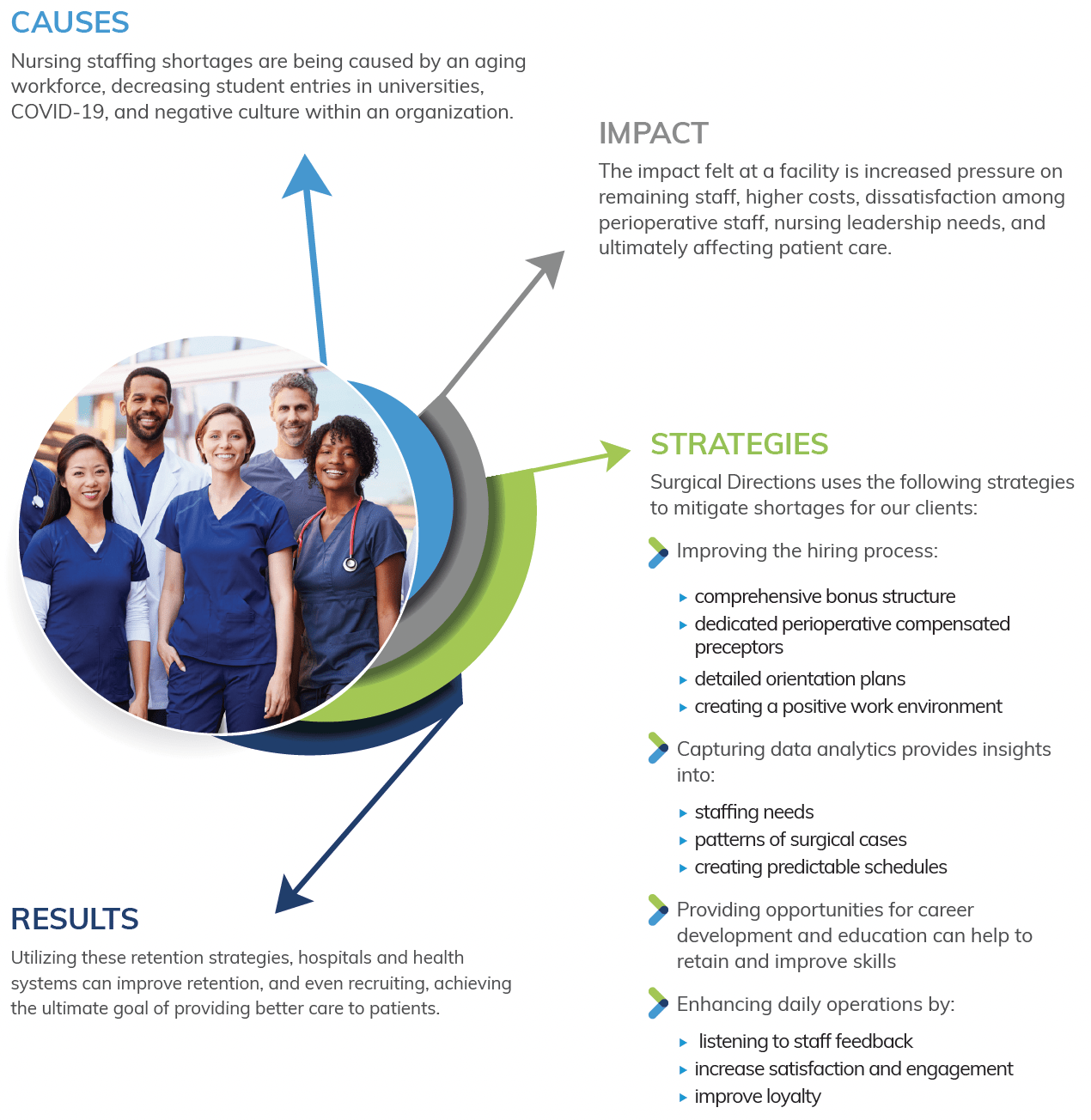
The shortage of nursing staff in healthcare is a major challenge faced by hospitals and health systems. With the increasing demand for healthcare services, coupled with an aging workforce, lower entries in universities and other factors, the shortage of nurses, particularly perioperative nurses, is at an all-time high. This shortage not only affects patient care but also affects the morale and work-life balance of the nursing workforce. The purpose of this white paper is to provide insights and strategies for mitigating the nursing shortage through effective retention strategies, with a focus on the perioperative nursing workforce.
Causes of Nursing Shortage
The nursing shortage is a complex issue, with multiple contributing factors. One of the main causes is the aging workforce, which is leading to a decrease in the number of nurses available to work. Additionally, there has been a decrease in the number of students entering universities to become nurses, which is compounding the problem. COVID-19 has further exacerbated the shortage by transferring nurses to areas where they are not as familiar, increasing the workload, and putting pressure on the work-life balance of nurses. The unavailability of supplies needed to care for patients, cost-cutting measures, variability in standard work, disruptive physician behavior, clinically unprepared patients, and a negative culture within the organization are also contributing factors to the shortage.
Impact on Hospitals and Health Systems
The nursing shortage is having a significant impact on hospitals and health systems. With fewer nurses available, there is increased pressure on the remaining staff, leading to burnout and turnover. The shortage also leads to higher costs as hospitals are forced to hire travelers or contract with agencies, which can be expensive. The lack of predictability in schedules can also be a significant source of dissatisfaction for perioperative staff. Furthermore, hospital clients are suffering from nursing leadership needs. Nurse leaders are in high demand, but with the unmanageable workload, increase in pay associated with interim positions and the burnout associated with COVID-19, they are in short supply. This is further exacerbates process improvement, optimization and ultimately patient care.
Retention Strategies
To improve retention there are four key strategies that should be considered as part of your work force management strategies:
- Improve the Hiring Process
- Capture Data Analytics
- Provide Career Development Opportunities
- Enhance Daily Operations
Improve the Hiring Process
Retention starts at the point of hiring and can be improved by providing a good bonus structure, dedicated perioperative compensated preceptors with a detailed orientation plan, and creating a positive work environment from the start. Training and feedback from preceptors, educators and management, as well as psychological safety training for all staff in the department, can help to encourage and nurture new hires and improve retention.
Capture Data and Analytics
Data analysis can play a key role in improving retention by providing insights into staffing needs and patterns of surgical cases, helping to level out staffing and provide predictable schedules. Using software, such as Merlin, can help hospitals and health systems to evaluate productivity targets and make improvements to operations, reducing gaps in the schedule and bringing elective cases during normal business hours.
Provide Career Development Opportunities
Providing opportunities for career development and education through clinical ladders and allocating funds for professional development and certifications can help to retain and improve the skills of the perioperative nursing workforce. Recognizing and acknowledging the achievements of staff as they move through the clinical ladder program can help to boost morale and improve retention.
Enhance Daily Operations
Finally, one of the most effective ways to improve retention is by listening to your staff and implementing things that would help them. By doing so, you can create a positive work culture that encourages employee satisfaction, engagement, and loyalty.
Listening to your staff involves gathering feedback and taking the time to understand their needs and concerns. This could involve
- Regular employee surveys
- Open-door policies
- One-on-one meetings
By listening to your staff, you can identify areas where you can improve working conditions, provide additional support, and make changes that will help them feel valued and respected.
Surgical Directions has helped our clients by:
- Optimize patients prior to day of surgery
- Develop standard work to streamline throughput
- Implement a collaborative daily review for proactive case management
- Establish surgeon, anesthesiologist and nursing daily operational oversite (3-legged stool)
- Design communication pathways designed for staff inclusion
Implementing changes that your nursing staff has requested not only shows them that their voice is heard and valued, but it also helps to build a culture of trust and collaboration. When people feel that they are part of a supportive, respectful work environment, they are more likely to be engaged, productive, and motivated to stay with the facility. Additionally, a positive work culture can also attract new nurses turning your retention strategy into a recruiting strategy through positive word-of-mouth in the community.



