The Road to Successful Perioperative Transformation for Bon Secours St. Mary’s Hospital
Bon Secours St. Mary’s Hospital is an acute-care facility with nearly 400 beds, located in Richmond, Virginia. According to Definitive Healthcare, the hospital’s patient mix is about one-third Medicare, one-tenth Medicaid, and the rest primarily privately insured. Richmond median incomes and home values are below Virginia state averages, 1 and the Richmond population is probably slightly more price sensitive for healthcare services than average for the state. Hospitals such as St. Mary’s must maximize efficiency and productivity to maintain margins in lieu of lifting prices.
Situation
The St. Mary’s Hospital leadership team was increasingly concerned about the hospital’s competitiveness compared with other local hospitals and newly built ambulatory surgical centers. St. Mary’s had been experiencing a steady decline in surgical case volume, and it was under growing financial pressure as its market share declined.
Compounding this problem, the leadership saw indications of staff coordination issues. A steady stream of complaints plus outright increases in staff turnover was evident. The administration felt the perioperative department was not appropriately coordinated internally across its many functions, such as pre-op, OR, pre-anesthesia testing (PAT), nursing, surgery, and anesthesia. Surgeons voiced complaints about OR access, and the Sterile Processing Department (SPD) was struggling to maintain appropriate quality standards.
The hospital leadership team considered issuing an RFP to find a new anesthesia group that could shore up the perioperative processes. But the team f irst reached out to Surgical Directions to identify any less-drastic but impactful changes that could be made to address the hospital’s issues.
Approach
Bon Secours engaged Surgical Directions to perform an assessment of perioperative services at St. Mary’s Hospital and determine the depth of issues that needed to be addressed. The Surgical Directions team was asked to provide recommendations along with a phased timeline approach to optimize staffing levels for surgery, anesthesia, nursing, staffing, and sterile processing.
Surgical Directions began the assessment with detailed data analysis spanning operational, financial, and market reports. Results were compared with our extensive benchmark database to determine opportunities. The team employed a variety of advanced analysis tools, opportunity heat maps, best-practice staffing models, and other techniques to identify opportunities.
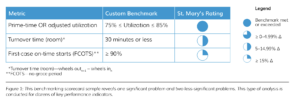
Additionally, the Surgical Directions team reviewed employee satisfaction surveys and other information highlighting cultural issues within the hospital and OR environment. The purpose of this data gathering and analysis was to gain insight into performance and key operating issues before conducting the on-site assessment. The client’s key performance indicators were compared with best practices from Surgical Directions benchmarks for similar institutions to help identify potential areas of improvement (see Figure 1).
Following the analytical phase, the Surgical Directions team held a final conference with key hospital and OR leadership to review the preliminary findings and provide recommendations for improving perioperative efficiency. The Surgical Directions team worked closely with hospital leadership to glean insight into how the hospital could build organizational consensus on change priorities.
Findings
Jointly the St. Mary’s and Surgical Directions team identified several opportunities for improvement:
- Boosting operational throughput
- Increasing OR prime-time access while balancing capacity with demand
- Establishing a collaborative governance structure
- Implementing a Co-Medical Director model
- Commencing block redesign and utilization maintenance
- Implementing an effective daily huddle
- Enhancing surgeon access and engagement
- Leveraging a growth strategy to increase case volume
- Increasing the engagement of proceduralists
- Leveling load staffing to align with surgeon block schedules
- Improving nursing and support-service engagement and retention
- Eliminating sterile processing issues—improving standardization, education, and turnover of instruments throughout the system
During the assessment, one-on-one interviews revealed that St. Mary’s Hospital had an OR director who was very much engaged and supportive of change. At the same time, the anesthesia department was respected for its clinical skills but wasn’t viewed as a valued partner with the hospital.
Senior leadership recognized the potential to achieve best-in-class status. However, surgical services were not organized to meet the needs of patients and surgeons. No effective perioperative governance structure existed, capacity was not optimally utilized, and systems were not in place to optimize patients’ clinical outcomes from the point of scheduling through 30 days of post-operative care.
Recommendations
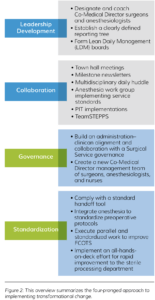
Assessment participants believed that the joint Surgical Directions and hospital leadership team prepared a workplan that would transform the perioperative department. The team worked in collaboration with an appointed multidisciplinary leadership committee to guide perioperative services from a fragmented, struggling department to a well-organized unit focused on patient care using a four-pronged approach: leadership development, collaboration, governance, and standardization (see Figure 2).
In addition, the team recommended several longterm strategies:
- Create a new administrative-sponsored leadership body: the SSEC (see sidebar)
- Implement a surgical growth strategy
- Overhaul block utilization guidelines
- Redesign the block schedule
- Restructure service line coordinators
- Align staffing with demand
- Upgrade scheduling processes
- Improve the patient preparation system
- Standardize day-of-surgery processes in pre-op
- Modify perioperative processes to improve throughput
- Establish dashboard reports to monitor perioperative performance
The hospital proceeded with an engagement during multiple months dedicated to improving the SPD. The off-site sterile processing facility handled reprocessing of instruments for all Bon Secours system facilities in Richmond.
What is a Surgical Services Executive Committee?
The Surgical Services Executive Committee (SSEC) is an administrative body comprising the leaders of the perioperative and surgical services affected by a change program. It provides critical governance oversight, helping to ensure the success of the overall program. Its scope of responsibility typically includes the following goals:
- Increasing surgeon satisfaction
- Improving OR performance
- Implementing tracking and analysis of quality metrics
- Enhancing efficiency
- Boosting profitability



