Last Updated October 21, 2024
The Struggling OR
Hospitals depend on the operating room (OR) to drive financial performance. In better-performing hospitals, surgical services account for more than 65% of gross revenue and up to 60% of operating margin. For many hospitals, however, poor OR performance makes the department anything but a financial powerhouse.
The mark of an underperforming OR is low utilization. Long gaps between cases lead to high operating costs coupled with low case volumes. Typically, volume is weak in both the main OR and non-OR anesthesia areas (NORAs). Low surgical services revenue ultimately weakens the hospital’s bottom line.
But while poor OR performance is deeply rooted, it is not inevitable
The key to turning around your surgery department is to understand the root issues that are leading to poor results. For the vast majority of underperforming ORs, the underlying problem is misalignment between physicians and OR leadership. The OR depends on surgeons and anesthesiologists, but excludes them from the decision-making processes that are critical to department success.
The solution is to put physicians in charge of your OR
Successful ORs have shown that physician leadership is the single most important factor in high performance. Surgeons and anesthesiologists are uniquely effective at solving the underlying problems that lead to poor utilization — and building a highly productive OR that drives strong revenue and profitability.
Does Your OR Look Like This?
Most hospital ORs are run by nursing management, often by a nursing director and nurse manager who are very skilled in their roles. Still, this management structure has two weaknesses:
- Surgeons and anesthesiologists have little say in OR management decisions, including decisions affecting scheduling, patient optimization, and clinical processes.
- Nursing leadership has responsibility for the department, but not the true authority needed to make many critical OR decisions.
The results are inaction and frustration
Troublesome efficiency problems become deeply entrenched.
Challenging issues in safety and quality remain unaddressed. Ultimately, mistrust grows between physicians, nurses and hospital administration.
The reality is that traditional OR management structures are unable to address the most pressing OR problems. Solving these problems requires a collaborative effort that engages physicians in a true leadership role.
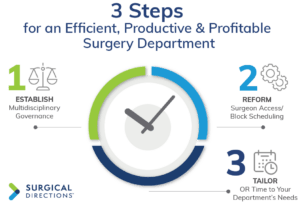
1. Establish Multidisciplinary Governance
Leading ORs nationwide have achieved effective physician leadership by creating a Surgical Services Executive Committee (SSEC).
An SSEC is a multidisciplinary governance committee for the OR. Effective SSECs bring together all four groups with an interest in the success of surgical services — surgeons, anesthesiologists, nurses and hospital administration.
Membership typically includes 7 to 10 active surgeons, plus key representatives from anesthesia, nursing and the executive suite. The committee should be chaired by one surgeon and one anesthesiologist who serve as co-medical directors of perioperative services.
Essentially, an SSEC is an “operational board of directors” for the OR. It is charged with overseeing the department’s operational, strategic and financial performance. SSEC members focus on specific OR problems and create policies and processes to improve perioperative efficiency and outcomes.
Executive support is essential
If there is one “secret ingredient” to the success of an SSEC, it is administrative support. Hospital executives must commit to honoring the decisions of the SSEC. This is not a risk. Hospitals nationwide have demonstrated that when physicians are put in charge of the OR, they make responsible and fair decisions about OR rules and resources.
2. Reform the Block Schedule System
In most hospitals, the SSEC’s top priority is to fix the block schedule system. An effective block schedule is the foundation of an efficient surgery department. Unfortunately, most OR block systems have several problems:
- Blocks are too short. Block time is allocated in short 4-hour units, creating obstacles to efficiency for both surgeons and staff.
- Blocks are group-owned. When blocks are assigned to surgical specialties or group practices, individual surgeons feel little urgency to use block time efficiently.
- Block rules are inadequate. In most hospitals, block schedule rules are weak or unenforced. Surgeon utilization is not monitored, and surgeons are allowed to cancel blocked cases on short notice with no repercussions.
These problems lead directly to low utilization. They also make it difficult for non-blocked surgeons to access the primetime schedule. A poor block schedule system also increases direct costs, as lateday scheduling pushes up staff overtime and call pay.
In most ORs, entrenched interests prevent leaders from fixing an ailing block schedule system. Strong SSECs, however, are able to command the broad-based support needed to create effective block schedule change. Key reforms include:
- 8-hour, 10-hour and 12-hour blocks. Longer blocks accommodate cases more efficiently and give surgeons the chance to have a productive OR day.
- Individual ownership. Surgeons who are assigned personal block time are personally responsible for using it effectively.
- Automatic block release. Specialty-specific release schedules give OR management the opportunity to fill up unscheduled block time.
- Utilization threshold. Surgeons are required to sustain a minimum block utilization rate, typically 75%.
Once block rules are strengthened, the SSEC monitors block time utilization. The committee removes block time from surgeons who fail to meet the utilization threshold two quarters in a row. This rewards high-utilization surgeons and ultimately improves overall utilization and OR case volume
3. Tailor OR Time to Your Department’s Needs
While strengthening the block system is critical, it is also important to build flexibility into the overall schedule. Again, a multidisciplinary SSEC is key to creating a well calibrated approach. Specific solutions include:
- Open rooms. When too much of the schedule consists of block time, non-blocked surgeons have trouble accessing the schedule. Often, younger surgeons are effectively “shut out” of the OR, creating long-term strategic problems. The SSEC should designate a portion of the schedule (typically 20%) as “open rooms” available for add-on elective and urgent/ emergent cases.
- Specialty rooms. Depending on your OR’s case mix and volume, it may make sense to establish dedicated rooms for key specialties. Some hospitals have created dedicated orthopedic ORs to support highvolume joint replacement service lines. Dedicated ORs with specialty nursing teams reduce operative and turnover times while improving surgeon satisfaction.
Dramatic Performance Turnaround
Leading hospitals demonstrate that physician leadership, block time reform and other changes can turn a poorly performing surgery department into a highly efficient, highly productive OR.
Surgical Directions recently worked with surgery department leaders at a large public hospital in the Southeast. The OR suffered from several performance problems, including low utilization, declining case volume and poor surgeon satisfaction.
We helped the hospital establish a strong SSEC, and then worked with the committee as it re-structured its block time system and OR schedule. Within one year, the OR experienced a dramatic turnaround in efficiency, productivity and profitability:
- Primetime utilization jumped from 38% to 68%
- Average monthly case volume increased 6.1%
- Revenue gains increased OR net margin by $3 million
Physician satisfaction increased markedly, as surgeons saw peer-led changes improving the operating environment while providing increased access to the OR schedule.
Are you ready to get started? Surgical Directions has worked with ORs nationwide to establish effective physician governance. To discuss your OR efficiency challenges and potential solutions, contact us today.