Superior patient-centered care crucial for complex outpatient procedures
About 2 years ago I was diagnosed with prostate cancer. As I researched the treatment alternatives, I became very concerned about the complications associated with traditional surgical prostatectomy or radiation. Then I learned that I might be eligible for an outpatient procedure: high-intensity focused ultrasound (HIFU). Although HIFU is relatively new in the US, it has been performed in Europe for decades. Studies show that, for the right patients, HIFU controls cancer as well as other interventions but with a much lower risk of complications.
After examining all the alternatives and speaking with several physicians, I decided to undergo HIFU at the Louisville Surgery Center in Louisville, Kentucky, in 2017. As someone who has worked with hospitals and ambulatory surgery centers (ASCs) for the past 35 years, I was impressed by the level of attention I received from John Jurige, MD, and his staff. They made sure I understood every step of the process and had everything I needed for a safe operation and a strong recovery, and they continue to follow up with me every 3 months.
My experience with this team got me thinking about the future of outpatient surgery. Traditionally, ambulatory surgery has consisted of relatively simple procedures performed on patients who need relatively little preparation and follow-up. However, now that more complex procedures are being performed in hospital outpatient departments and ASCs, I believe healthcare providers must rethink their patient engagement models. They need to develop new ways to communicate with patients, prepare them for their procedures, track long-term outcomes, and maintain ongoing relationships.
Patient engagement pathway
Dr Jurige has been performing prostate HIFU for more than 12 years. “In this procedure, we use a transrectal probe to target ultrasound energy on cancerous tissue in the prostate,” he says. “Although HIFU does require patients to have a general anesthetic, the procedure is relatively noninvasive, and the side effects are minimal.”
Before the Food and Drug Administration approved HIFU for prostate tissue ablation in 2015, Dr Jurige performed the procedure in ASCs in Canada, Mexico, and the Caribbean. Because both he and his patients traveled across borders, he developed systems for coordinating the entire patient experience.
“I learned that we needed to have systems in place to help patients with things such as travel, accommodations, and transport to and from the ASC,” Dr Jurige says. “So going beyond patient education, we really needed to provide a concierge level of patient communication.”
The team’s communication platform takes advantage of several different technologies. For example, patients may have an online consultation with Dr Jurige via an electronic medical record portal that complies with HIPAA (the Health Insurance Portability and Accountability Act of 1996).
“Patients can take part in the consult through their laptop, tablet, or even smartphone,” he says. “It lets them see me, hear my voice, and listen to my explanation of the procedure, recovery, and potential outcomes. With the exception of a physical examination, I can accomplish the same thing with the online consult that I can in a face-to-face setting, and I think it’s a very good method for establishing, at least initially, a doctor-patient relationship.”
Patients can also use the portal to exchange secure emails with the care team. In addition, all patients are given secure business cell phone numbers for Dr Jurige and the nursing staff. They can call or text the team to ask questions, clarify instructions, get laboratory test results, or just seek reassurance. “The ability to get a direct and prompt interaction with me or my staff really allays a lot of anxiety for both patients and their families,” Dr Jurige notes.
But isn’t personally responding to patient calls and texts time-consuming for a surgeon? According to Dr Jurige, it’s actually efficient. “The alternative would be that the patient contacts the office, speaks to an assistant, and is transferred to a nurse. Eventually the message gets to me, and then I would use the reverse passageway to try to communicate something back to the patient.” Not only is that approach lengthy, it creates many opportunities for miscommunication.
“I don’t find direct patient access to be time-consuming because I know there’s an efficiency built into it,” Dr Jurige says. “If the patient has a question for me about the procedure or about his cancer, I can respond to him in one step. For me, the ability to take care of these things directly with the patient is a timesaver, and I think it enhances the relationship.”
Like all HIFU patients, I received a 16 Fr Foley catheter that remained in place for nearly a week. I had a lot of questions: How often do I have to clean the collection bag? Can I wear the catheter to work? What amount of skin irritation is normal? Why am I seeing blood? The ability to ask my surgeon and nurses about these concerns gave me peace of mind and helped me better manage my own recovery.
Careful follow-up is also an important element of Dr Jurige’s patient engagement strategy. After my HIFU treatment, he called me twice in the first few days post-procedure. Now, practice staff contact me every 3 months to arrange for laboratory tests and verify completion. Dr Jurige texts me to comment on the results of each test and note any next steps.
Dr Jurige’s practice contributes to a prostate HIFU registry that tracks oncologic outcomes, complications, and quality-of-life indicators, so regular follow-up is essential. “HIFU is just now beginning to have widely accepted insurance coverage, and in some cases, it is still a patient-pay procedure,” he says. “In that regard, we do like to extend additional patient services that provide continuity of care and peace of mind for patients.”
According to Dr Jurige, this comprehensive communication model facilitates the delivery of personalized care. “Some patients have a lot of concern about one particular potential side effect of the procedure—such as preservation of erectile functioning or preservation of bladder functioning—while for others, the main concern above all else is cancer eradication,” he says. “I think the most important thing about our system is that it lets us get to know the personality of the patient, and it provides flexibility and adaptability based on the needs of the patient and his family.”
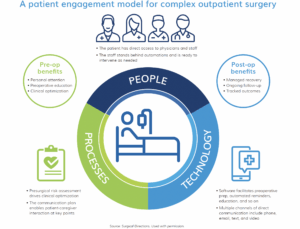
People, processes, and technology
A key to success for any procedure is making sure the patient is clinically optimized before the date of surgery. This principle is even more important when performing advanced procedures in an outpatient setting. Increasingly, hospital outpatient departments and ASCs are using patient engagement software to support presurgical optimization.
Most software systems are able to send automated patient reminders about appointments and procedure times, push educational videos and other content, and deliver preoperative instructions on things like diet and bowel prep.
In my experience, most patients love patient engagement software because it allows them to manage their operations from their smartphones. In fact, some healthcare organizations in economically stressed communities give smartphones to surgery patients. The cost of the device is minuscule compared to the benefits in patient optimization and communication efficiency.
The most advanced patient engagement systems also include capabilities for preadmission screening. Typically, the software portal features a presurgical questionnaire designed to assess patient risk based on demographics, medical history, and other factors.
According to Thomas Blasco, MD, senior medical director for Surgical Directions, patient engagement software provides new opportunities for optimizing the preadmission screening process. “Preadmission screening can certainly be done verbally, but the logistics can be problematic,” he says. “It is much easier when patients have the opportunity to pre-answer the questions through the software. A nurse can then follow up by phone to verify the patient’s responses, determine patient acuity, and route the patient for appropriate preoperative management.”
Dr Blasco believes that software-driven education and communication can help support patients who are scheduled to undergo a major procedure like joint replacement in a day-surgery setting.
“The patient may be quite worried because all [his] friends have had their joints done in the hospital, with narcotic-based pain control and 4 days in a skilled nursing facility,” he says. For these patients, the additional support provided by a robust digital engagement platform can aid peace of mind and contribute to a good outcome.
“And joint replacement is just the start. People are talking about doing neurosurgery and cardiac surgery as outpatient procedures,” Dr Blasco says. “There is no way we will be able to do these procedures in ASCs without versatile systems for engaging and managing patients and maintaining ongoing connectivity.”
Dr Blasco offers one caveat for organizations that want to target software-driven patient engagement: “It can’t all be automated—you have to have people there to back up the software. You can use technology to support the overall pathway, but you still need a carefully choreographed process that may require immediate patient access and direct provider intervention.”
Dr Jurige and his staff have a well-established HIFU program, and they provide education to other surgery centers that want to offer this procedure. The training covers physician education on how to perform the procedure, plus specific setup, tear-down, and disinfection processes for prostate HIFU.
“Centers interested in providing the procedure can purchase or lease a mobile HIFU system that integrates multi-parametric prostate MRI imaging,” he says. “Other than the ablation system, very little equipment is needed beyond a basic urological outpatient procedure setup.”
Changing mindsets
Dr Jurige believes it’s important for surgery leaders to change the way they think about outpatient surgery.
“So many advanced procedures can now be done with minimal blood loss and minimal pain medications that a traditional inpatient stay is unnecessary,” he says. “But if you are going to do advanced procedures in an outpatient surgery department or an ASC, your mindset needs to shift away from the way we prepare for minor procedures.”
The focus should be on building systems around the needs of patients. “Putting the right patient management and patient engagement systems in place is key to extending and broadening the capabilities of an outpatient surgery center,” Dr Jurige says.
Reference
Guillaumier S, Peters M, Arya M, et al. A multicentre study of 5-year outcomes following focal therapy in treating clinically significant nonmetastatic prostate cancer. Eur Urol. 2018;74(4):422-429.



