Introduction
An inefficient OR that does not provide surgeons sufficient access to its services can result in a restricted ability to schedule cases. This limitation can lead to problems for patients, and for surgeons it can create barriers to using a particular facility.
Patients may be at higher risk for poor outcomes, including surgical site infections, longer recovery times, and higher post-op readmission rates. Surgeons, meanwhile, might experience delayed starts, reduced case volume, excessive idle time with suboptimal block utilization, and higher frustration levels.
Inefficiency and poor OR access can stem from a host of issues, from cumbersome scheduling practices to careless use of reserved OR block time. However, using the appropriate strategies, hospitals can address these issues by providing optimal surgeon access and enhancing overall efficiency.
Following five basic guidelines can help your hospital provide suitable surgeon access to your ORs:
- Preparing patients for surgery can help ensure cases are ready to start when the surgeon arrives and promote best outcomes for patients.
- Allocating block time appropriately helps improve case flow through the OR and enables surgeons to efficiently plan their schedules.
- Optimizing OR utilization can minimize downtime, which helps enhance surgeon productivity and boost facility and physician revenue.
- Simplifying the scheduling process can mitigate many barriers and irritations for surgeons when they work with hospital ORs.
- Seeking surgeon input gives surgeons a forum to raise issues of concern and contribute to the governance of the OR.
Implementing these guidelines helps improve patient outcomes while also protecting the bottom line for both surgeons and hospitals.
Prepare Patients for Surgery
Patients often need pre-surgery tests such as a blood test or an electrocardiogram to make sure they are healthy enough for the procedure. Preparing a patient means helping to ensure the patient has been evaluated and tested as needed and the results have been reviewed by the primary care physician, anesthesiologist, or both. Ideally, test results should be reviewed three to four days before the procedure so that an abnormal test result can be managed, as needed. To determine whether patients are being sufficiently prepared, review surgeries that have been cancelled within 24 hours of the scheduled time. A common reason for a surgery cancellation within 24 hours of the scheduled time is the failure to conduct appropriate preadmission testing. Making sure a patient is ready for surgery can reduce the chance that the procedure will be cancelled or delayed.
Backfilling, or scheduling another surgery to replace the cancellation, is often not possible in such a short amount of time. Day-of-surgery testing that could have been accomplished prior to surgery is expensive, contributes to delays, and runs the risk of an incomplete evaluation of the results. When preadmission testing does not occur, it is often because of a breakdown in communication between the surgeon’s office and the hospital’s perioperative staff.
For example, if a patient has any type of a cardiac condition, that information should be conveyed to the surgeon and the hospital’s surgical staff. Together, they need to make sure the appropriate tests are performed ahead of time and the patient is medically optimized prior to the procedure. Establishing formal oversight of the preadmission process helps address this issue. Hospital teams and anesthesiologists need to develop preadmission testing guidelines for staff physicians’ offices and the hospital. A healthy patient with no known conditions might require no preadmission testing, while a patient with high blood pressure and obesity might require multiple tests. Using a testing grid guideline facilitates identifying patients who also need a formal preadmission testing visit—in addition to phone and virtual screening processes—for medical optimization and a perioperative workup. A defined and structured preparation process can help prevent delays and cancellations.
Allocate Block Time Appropriately
Hospitals must have an adequate amount of blocked and open OR time—both for add-on cases and for surgeons who do not have formal block time. If this time is used inefficiently, hospitals and surgeons might lose revenue and create frustration for the physicians and OR staff.
The problem is that block time is often underused. For example, a surgeon might have five hours of OR time reserved three days a week but use only 30 percent of that time. Or a surgeon might schedule a vacation and not inform the hospital until a day or two before the vacation begins, reducing the opportunity to back-fill that open time.
Establish targets for surgical block utilization rates. Generally, surgeons should use 90 percent of their block time. That block time usage should then be evaluated using a scorecard for each surgeon. Most importantly, surgeons should understand that if they do not meet block utilization rates, they could lose the reserved time. OR directors should be ready to designate that block time to surgeons who do not have any reserved time but have enough volume to be granted block time.
Optimize OR Utilization
Keeping an underutilized OR open is a waste of clinical, staffing, facility, and supply resources. But not providing sufficient openings can frustrate surgeons and reduce revenue for the hospital. Finding the right balance can be challenging.
The threshold for OR utilization should be an adjusted rate of 75 percent. In other words, if your hospital has 10 ORs open 10 hours a day, and the 10th OR is used 75 percent of the time, utilization is appropriate. If the 10th OR is in use 85 percent of the time, however, another OR might be necessary. With 85 percent utilization, enough time isn’t available to add another surgery in existing ORs because that 15 percent of unused time is spread over several rooms. One room may have 10 minutes of unused time, another may have 20 minutes, and so on. Not enough time is available in any one room to complete a procedure.
Many single hospitals and small health systems may use spreadsheets to manually collect and analyze utilization data. But this methodology may be prone to error, which can lead to mistrust among the surgeons. If possible, these organizations should instead use operational data, electronic medical records, and business intelligence software to calculate optimal and accurate OR utilization rates.
Simplify the Scheduling Process
An inefficient OR scheduling process is often indicated by poor scores on patient and surgeon satisfaction surveys. In the extreme, poor processes can prompt surgeons to seek other hospitals to perform their procedures. In addition, the hospital can waste a significant amount of time and human resources when making multiple calls to surgeons’ offices to find incomplete and missing information.
A centralized scheduling process is key to enhancing efficiency and getting procedures scheduled in a reasonable period of time—such as two to three weeks instead of two to three months. One of the challenges is that each physician’s office uses different processes, and some are more efficient and complete than others.
Identify physicians’ offices with poor scheduling practices and those with efficient practices. Then, using a peer-to-peer technique, transfer those efficiencies to the offices that need help. You might discover, for example, that in efficient offices, staff members have a better understanding of clinical terms, which can help to speed up the process and reduce errors. Augmenting training, or providing supporting educational materials, can help improve understanding of terms.
One-time visits to poor-performing offices can also uncover issues that are causing inefficiencies. For example, staff members in these offices might have poor computer skills and rely heavily on manual processes, which can increase the time and error rate in scheduling a case. In some instances, these types of problems can be remedied by showing staff how to maximize the use of computer and non-computer-based productivity tools, such as sending a document electronically rather than using a fax machine.
Engaging with physician schedulers and office managers—for example, by hosting a welcome or appreciation lunch—can help to build trust, solidify relationships, and create peer-to-peer networks. Trying to make the scheduling process easier for surgeon schedulers is critical. The more you can work with a physician’s office to help improve the process for the scheduler, the more likely the staff is to schedule with your hospital.
Seek Surgeon Input
Solutions in healthcare are often found through effective and sincere collaboration. Including physicians and staff members who are on the front line is critical to the success of any collaboration. Because inefficient block time can be one of the greatest impediments to physician access, creating a body of authority—through an OR governing committee—to review block time utilization can provide the best results. This committee should be both multidisciplinary and interdisciplinary, including not only practicing surgeons but also representatives from anesthesia, nursing, and administration.
Many committees will benefit from establishing standardized definitions for key terms, such as utilization and management, block release time, and methodology for block allocation. No two hospitals measure utilization in the same way. For example, if a surgeon’s block time is 12 pm to 3 pm, but the surgery lasts until 5 pm, do those last two hours count toward the surgeon’s utilization? One hospital might count the hours that extend beyond a surgeon’s blocked time toward utilization, while another hospital might not.
The physicians who serve on the block utilization committee should act as champions within and for the committee, seeking input and obtaining buy in from their colleagues on new OR rules, methods, and practices regarding the OR. This collaboration helps to further establish a relationship of trust between the hospital and surgeons.
Case Study: How Bon Secours St. Mary’s Hospital Helped Improve Surgeon Access and OR Performance
Bon Secours St. Mary’s Hospital is an acute-care facility with nearly 400 beds, located in Richmond, Virginia. According to Definitive Healthcare, the hospital’s patient mix is about one-third Medicare, one-tenth Medicaid, and the rest primarily privately insured.
Richmond median incomes and home values are below Virginia state averages, 1 and the Richmond population might be slightly more price sensitive for healthcare services than the state average. Hospitals such as St. Mary’s must maximize efficiency and productivity to maintain margins instead of lifting prices.
Situation
The St. Mary’s leadership team was increasingly concerned about the hospital’s competitiveness compared with other local hospitals and newly built ambulatory surgical centers. St. Mary’s had been experiencing a steady decline in surgical case volume, and it was under growing financial pressure as its market share declined.
Compounding this problem, the leadership saw indications of staff coordination issues. Surgeons voiced complaints about OR access, and an increase in staff turnover was evident.
The administration felt the perioperative department was not appropriately coordinated internally across its many functions, such as pre-op, OR, preanesthesia testing (PAT), nursing, surgery, and anesthesia.
Discovery
In partnership with Surgical Directions, St. Mary’s conducted a benchmarking study to assess the hospital’s OR performance relative to peer facilities. The findings showed a couple of areas with significant performance gaps (see Figure 1). After analyzing data and conducting numerous surgeon and staff interviews, the Surgical Directions team developed a series of process improvement recommendations.
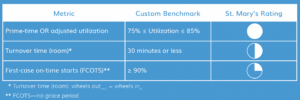
Figure 1: This benchmarking scorecard sample reveals one significant problem and two less-significant problems. This type of analysis is conducted for dozens of key performance indicators.
The goal of these recommendations was to enhance surgeon access and OR performance in the following ways :
- Boosting surgical case throughput (OR utilization)
- Redesigning the surgical blocks overall
- Increasing OR prime-time access while balancing capacity with demand
- Establishing a collaborative governance structure that provides a mechanism for surgeon input
- Redesigning and implementing a new pre-anesthesia testing process to help improve first-case on-time starts (FCOTS)
- Leveraging a growth strategy to increase case volume
Results
Following the recommendations paid dividends. In virtually every performance area measured, the hospital moved rapidly toward specific operational improvement objectives over its current benchmarked levels (see Figure 2). The result of the performance improvement has been a significant increase in both daily case volumes and overall surgeon satisfaction. By eliminating various barriers to access, St. Mary’s Hospital has made great strides in better serving the needs of both the community and its surgeons.2

Figure 2: Team-defined operation improvement goals reflect significant improvement over the baseline observed during the analysis phase.
Start Improving Access and Efficiency Today
As the healthcare industry becomes more competitive, hospitals need to do everything possible to improve access to the OR for surgeons and maximize overall efficiency. Achieving these goals is vital for increasing performance and sustaining revenues. By focusing on a few guidelines, your hospital can optimize the value of ORs while helping improve surgeon satisfaction and patient satisfaction as well as strengthening its reputation as a reliable, efficient facility for surgical procedures.
Resources
1 City-Data.com. Retrieved from www.city-data.com/city/Richmond-Virginia.html.
2 For the complete case study, visit www.surgicaldirections.com/resource/bon-secours-st-marys-hospital/



